Arrhythmias in Single Ventricle Patients
Dr Sarah Boynton –Paediatric Cardiology Registrar
Heart Unit –Birmingham Children’s Hospital
The heart is a powerful pump, which tries to satisfy the body’s need for oxygen at all times. It does so by making the filling chambers (atria), the valves and the pumping chambers (ventricles) work in perfect harmony. The key to achieving this is the heartbeat (electrical activity). In people with a single ventricle a normal heart beat and synchrony of all its components is even more important than in people with a normal heart.
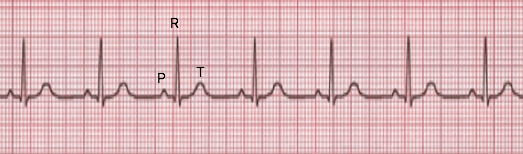
The normal heart beat:
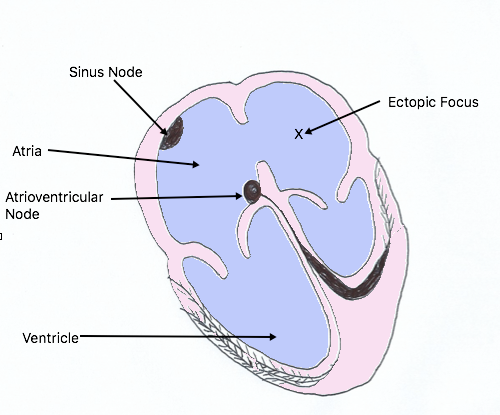
The heart beat originates in the top part of the right sided filling chamber (sinus node) and then spreads all over the filling chambers to reach a small area between the filling and pumping chambers (the atrioventricular node) from where it eventually spreads to the pumping chamber forcing them to eject the blood vigorously to the body. There is then a recovery phase where the heart relaxes and blood that has returned from the lungs to the heart passively again fills the ventricle.
Making the filling chambers contract before the pumping chambers allows the heart to be more efficient, as it will eject some 15% more blood per heartbeat. This is particularly important during exercise when the heart rate increases as a response to the increased demand of the body.
The various phases of the cardiac cycle can be seen on an ECG. Atrial contraction is represented by the p wave, the time delay at the atrioventricuar node is shown by the PR interval, the contraction of the ventricles is depicted as the R wave and relaxation by the T wave. When the electrical system is functioning normally, with normal time delays it is referred to as sinus rhythm. When the heart beats too fast it is referred to as tachycardia and too slow it is bradycardia. These can be sinus (as in the normal electrical system) or none sinus (as when the normal electrical system has failed).
The heart rate goes up and down in order to meet supply and demand of the body. It speeds up during exercise and slows down during inactivity.
Maintaining normal sinus rhythm is important for the function of the heart, if it is beating too fast or too slow for prolonged periods of time it can be detrimental to the function of the heart muscle. If sinus rhythm is interrupted then the heart may not be able to meet the demands of the body.
If the sinus node is damaged or ceases to function properly other parts of the heart can take over the role of the pacemaker, however the rate at which electrical signals can be generated varies depending upon the location of the “new pacemaker”. If the new region is high in the atria or at the level of the junction (AV node –junctional rhythm) then the rate of contraction generated is often sufficient to meet the body’s demands. If the rate generated by this new pacemaker is too slow and the ability to increase the heart rate during activity is lost then this presents with breathlessness and easy fatigue even on minimal tasks. Also if the rate is too slow then the function of the pumping chamber can deteriorate exacerbating symptoms. Ectopic areas can also develop within the heart and act as new pacemaker, these can generate electrical signals which are much faster than the sinus node and can result in very fast heart rates which can also affect cardiac function and output.
The heart rhythm is monitored in outpatients by performing ECG’s. If a loss of sinus rhythm is detected then further investigations can be carried out. The first is usually a Holter monitor. This is a small portable box that continually records the heart rate and rhythm over 24 -48 hours. An exercise tolerance test can also be carried out. ECG leads are positioned in a similar way to the standard 12 lead ECG then you will be asked to exercise on a treadmill or in some places on an exercise bike, the intensity of exercise performed is slowly increased and the ECG rate and rhythm are recorded. This investigation tests both your ability to exercise before becoming fatigued and it also shows the ability of the heart to increase its rate in response to exercise. Saturations and Blood pressure can also be monitored during exercise.
If during these investigations the heart rate is found to be too slow or the chambers are contracting out of sync to each other and affecting the function of the heart then an operation to fit a pacing box and leads can be performed. Pacing leads are fitted to the surface of either or both the ventricle and the atrium and these are then attached to a box ,which is placed under the skin in either the abdomen or on the chest. The box then generates electrical signals initiating contraction at a programmed rate. Once you have a pacemaker fitted you will also need to be followed up in a pacing clinic, which monitors the battery life of the pacing box and the integrity of the pacing leads.
The electrical system can also malfunction resulting in the heart beating too quickly, which again can lead to problems with heart function or an inability for the heart to pump out enough blood to meet the demands of the body resulting in collapse. These fast rhythms are often collectively referred to as supraventricular tachycardias with rates over 200 beets per minute. These can present with palpitations (an awareness of your heart beating very fast) or with breathlessness, chest pain, tiredness or collapse.
The arrhythmia may be detected on the ECG in outpatients but more often a history of symptoms will prompt the need for longer term monitoring in the form of a Holter monitor, which can continually record your heart rate and rhythm for up to a week. If your symptoms are occurring less frequently you can be fitted with an event / loop recorder. If you have symptoms you press the button and the loop is stored from a few seconds before you pressed the button for a programmed amount of time. This type of monitor can be worn for up to 30 days. If symptoms are less frequent but still problematic the option of having a Reveal device fitted may be discussed. This is a more invasive option as it is inserted just under the skin over the heart and it can remain in place for up to three years.
If a fast rhythm is detected during your follow up the first line of treatment is with medication. If medication does not control the arrhythmia or it is poorly tolerated then the option of an electrophysiological study and ablation may be discussed. This is a catheter procedure used to “map” the electrical activity of the heart and to find a focus that is responsible for the fast heart rate. If a focus is found it may then be possible to ablate (burn or freeze) the area responsible for generating the fast rhythm.
Summary:
The normal heartbeat makes the filling and the pumping chambers work in harmony to supply the body with oxygen at rest and during exercise. An abnormal heartbeat can be detected with an ECG or longer-term monitoring. Pacemakers can be used to address slow or uncoordinated heart beats and medicines or catheter procedures can be used to address too fast a heartbeat.
Page uploaded September 2023