Diagnosis
Learning that your baby has a complex heart problem can be frightening and leave you feeling very alone.
Here we hope to help you understand your baby’s heart problem and explain some of the choices you have been given. If at any time you would like to chat through the information you have been given, do not hesitate in giving the LHM team a ring on 0121 455 8982.
There are many different congenital heart defects (CHDs). A ‘congenital’ problem is one that a baby is born with. Some are minor defects such as small holes in the heart which may not need any treatment. Others, although more serious, can be corrected with an operation.
Contents
(Clicking the links below lets you jump to the difference sections)
How the diagnosis of single ventricle heart disease is made
There are two main opportunities for a diagnosis of complex heart disease to be made – either before or after birth.
Antenatal diagnosis
In many cases it is now possible to make a diagnosis of a single ventricle condition when a pregnant woman undergoes her 16 – 20 week ultrasound scan. Scans before this stage of the pregnancy are unlikely to detect problems because the baby’s heart, lungs and other organs are not big enough to be seen clearly.
A sonographer (the member of staff who scans mothers to look at the baby) will be looking to see that the baby’s heart has four chambers, and two major crossing blood vessels leaving the heart. If there is any doubt that the baby has a normal heart or other organs the sonographer will seek a second opinion from the obstetrician or fetal medicine doctors (doctors who specialise in looking at unborn babies).
If a problem with the heart is seen clearly, the obstetric team will refer the family to a specialist in this field, a fetal cardiologist (a heart doctor who specialises in looking after unborn babies). If a complex condition is confirmed, the cardiologist and the obstetric team will talk to the family about the diagnosis and the possible treatments. They will offer further tests, such as amniocentesis, to see if the baby has any unseen problems with their genetic picture (to see if the blueprint of the baby has a fault – for example, something like Down’s syndrome). For more information on antenatal tests speak to your midwife.
Once all of the tests have been completed the family will be given the opportunity to discuss the future for their child. The team will support the family whilst they make their decision either to continue with the pregnancy or to end the pregnancy through termination.
Most babies with a single ventricle condition grow well in their mother’s womb. They are usually born between 38 and 40 weeks of pregnancy. It is only after birth, once their fetal circulation changes (see Fetal Circulation) that their defects begin to affect their bodies.
For more information on antenatal diagnosis refer to Antenatal Information.
Postnatal diagnosis
As long as the ductus arteriosus remains open, it is often difficult to detect that a newborn baby has a problem with its heart. (See Fetal Circulation).
As the ductus arteriosus closes the baby will become breathless and sweaty, sleep more and drink less milk. This can happen while the baby is still in hospital and may be detected by the midwife or doctor as they do their post-delivery checks or within a few days of going home when the midwife or health visitor should notice that the baby needs to see a doctor.
Once the baby has been referred to a paediatrician (baby doctor) tests will be done to try and find out what is causing the problem. Medicine called Prostaglandin will be given to the baby to try and keep the ductus arteriosus open, as this will keep the baby alive until treatment decisions can be made. (See Fetal Circulation).
The baby will be transferred with a medical team to the nearest hospital that treats congenital heart defects. Here the baby will have an ultrasound scan (echocardiogram or echo) similar to the scans done in pregnancy. The specialist heart team will be able to see what the heart looks like and will be able to make a diagnosis.
Questions commonly asked at the time of diagnosis
What causes the heart to form this way?
As yet the causes of single ventricle heart conditions are unknown. They cannot be linked with mild drinking or the taking of ‘over the counter’ or most prescribed medications. There are some indications that these conditions can be linked to heavy smoking, alcohol or drug abuse. Anyone with diabetes has an increased risk of having a child with a heart condition. It is very likely that one or more abnormalities are present before the third month of pregnancy but they may become more obvious as the heart is growing through the second half of the pregnancy. Heart abnormalities can be present in babies who have other congenital problems, for example, genetic disorders like Edwards’ syndrome or DiGeorge syndrome (22q Deletion).
Why was the problem not detected during pregnancy?
It is possible to detect single ventricle heart disease during pregnancy but it may not be obvious during scans due to the size or position of the baby. In some cases the condition can become more evident later in pregnancy after the routine scans have been performed.
Why is the condition treatable but not correctable?
Doctors have developed a way of bypassing the malformations within the heart so that blood can circulate around the body but they are unable to make a ventricle, so even following surgery the heart will only have one working pump rather than the two seen in a normal heart.
What does palliative mean?
Palliative treatment means that the treatment is unable to cure the problem. In the case of the treatment for a complex heart problem it means that the treatment can bypass but not cure or totally correct the problem.
Can my baby have treatment anywhere in the country?
Most – but not all – congenital heart centres around the country offer surgery for these conditions. It may be necessary for your baby to move hospital to receive treatment. This would be discussed with you at the time of diagnosis.
The normal heart
Understanding the normal flow of blood through the heart can be daunting so here we have described it in two ways.
The heart is a clever pump. Its job is to collect and send blood to different parts of the body. Blood contains all the things we need to make energy: oxygen, nutrients (food) and water, which it takes to every part of the body so that every part of the body has the energy it needs to work, grow and repair.
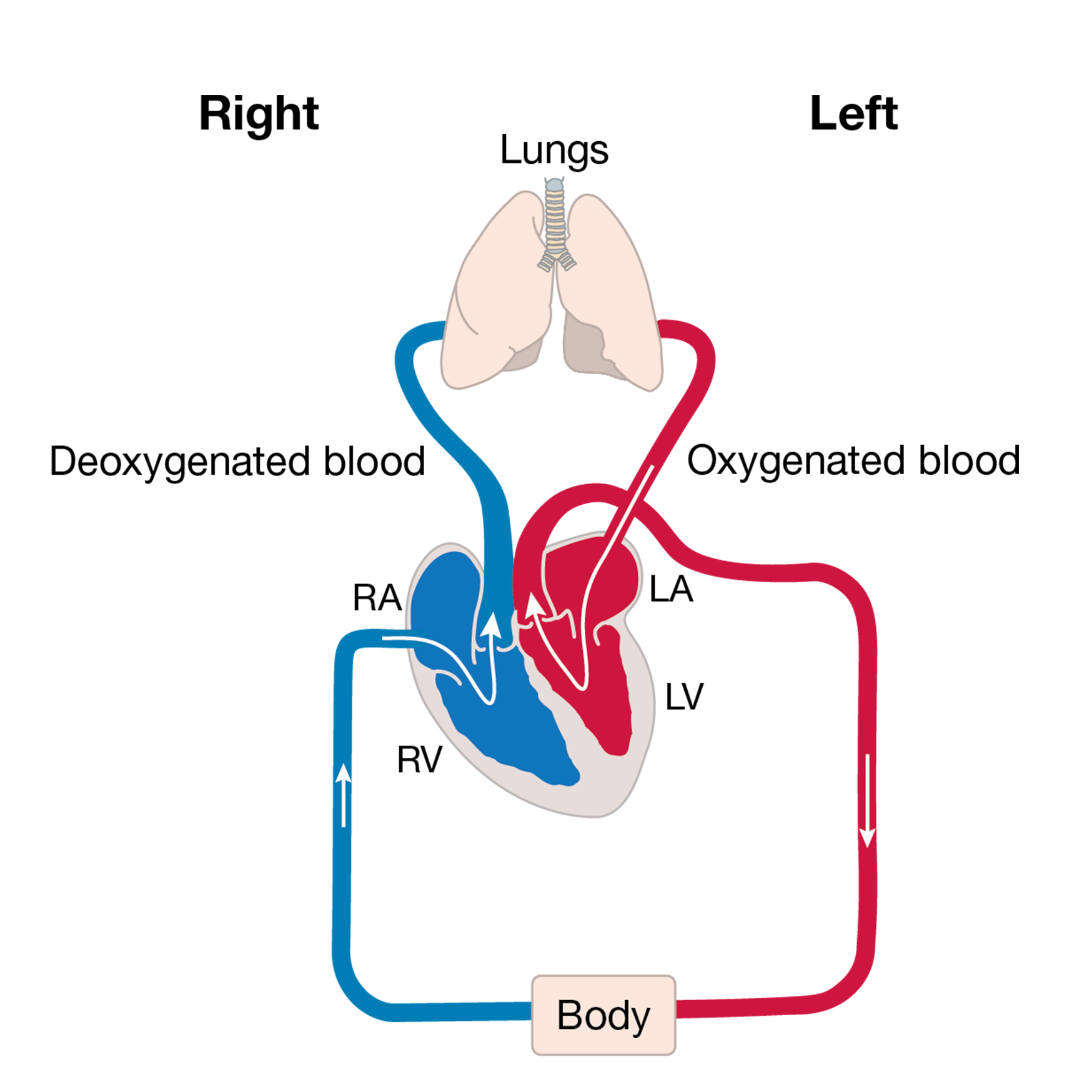
The body’s circulation has red blood that is filled with oxygen and blue blood that is empty of oxygen.
The heart has two sides. The right side’s job is to collect blue blood from the head, neck and body into the top right chamber (the right atrium). It then passes into the bottom chamber (the right ventricle) which pumps the blood to the lungs. The lungs do their job and pass oxygen into the blood; this turns the blood red. This oxygen-filled blood then needs to be pumped around the body by the heart. The red blood is collected in the top left chamber (the left atrium) and then passes to the lower chamber (the left ventricle) that pumps the blood out of the heart and around the body.
The body uses all the oxygen in the blood, turning the blood blue, and then sends it back to the right side of the heart to start the journey all over again.
The following paragraphs explain the heart again but use more of the terms you may hear from your medical team and the picture looks more like a real heart.
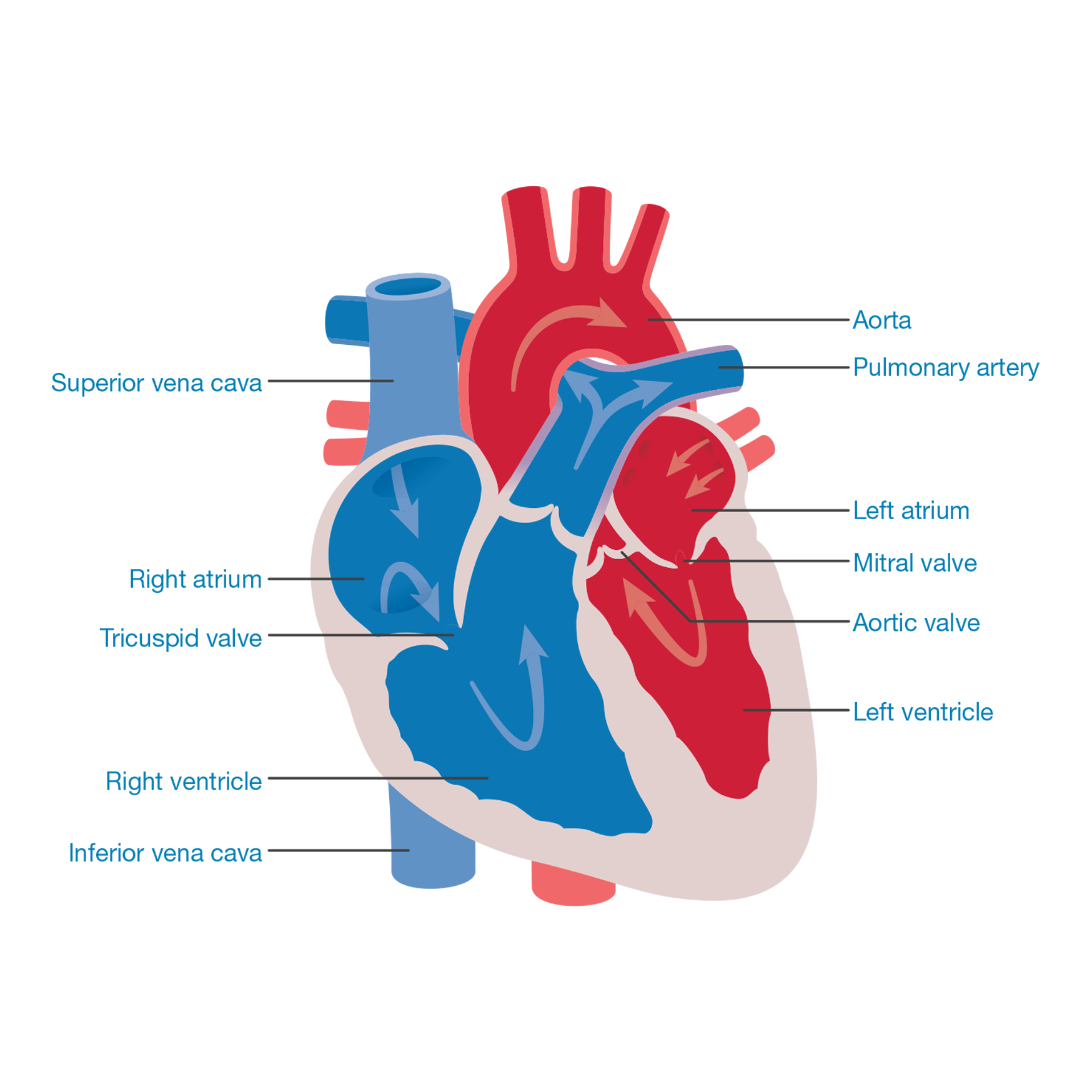
This is how the journey begins: blood returns from the body, via the superior vena cava and the inferior vena cava, to the right side of the heart into a collecting chamber (right atrium). This blood has a bluish tinge (blue blood) because the body has taken (extracted) all the oxygen from it (deoxygenated blood).
The blood passes through a valve (tricuspid valve) into a pumping chamber (right ventricle), which then pumps the blood to the lungs via the lung arteries (pulmonary arteries).
As the blood passes through the lungs it picks up oxygen: this turns the blood a red colour (oxygenated blood). This blood flows to the left collecting chamber (left atrium) and then passes through a valve (mitral valve) to the left pumping chamber (left ventricle).
The left ventricle then pumps blood to the body through a valve (aortic valve) via the main body artery (aorta).
The body uses the oxygen from the blood to help make energy. As the oxygen is used up, the blood takes on a blue colour and needs to return to the lungs to collect more oxygen. The journey then starts again.
The circulation before birth (fetal circulation)
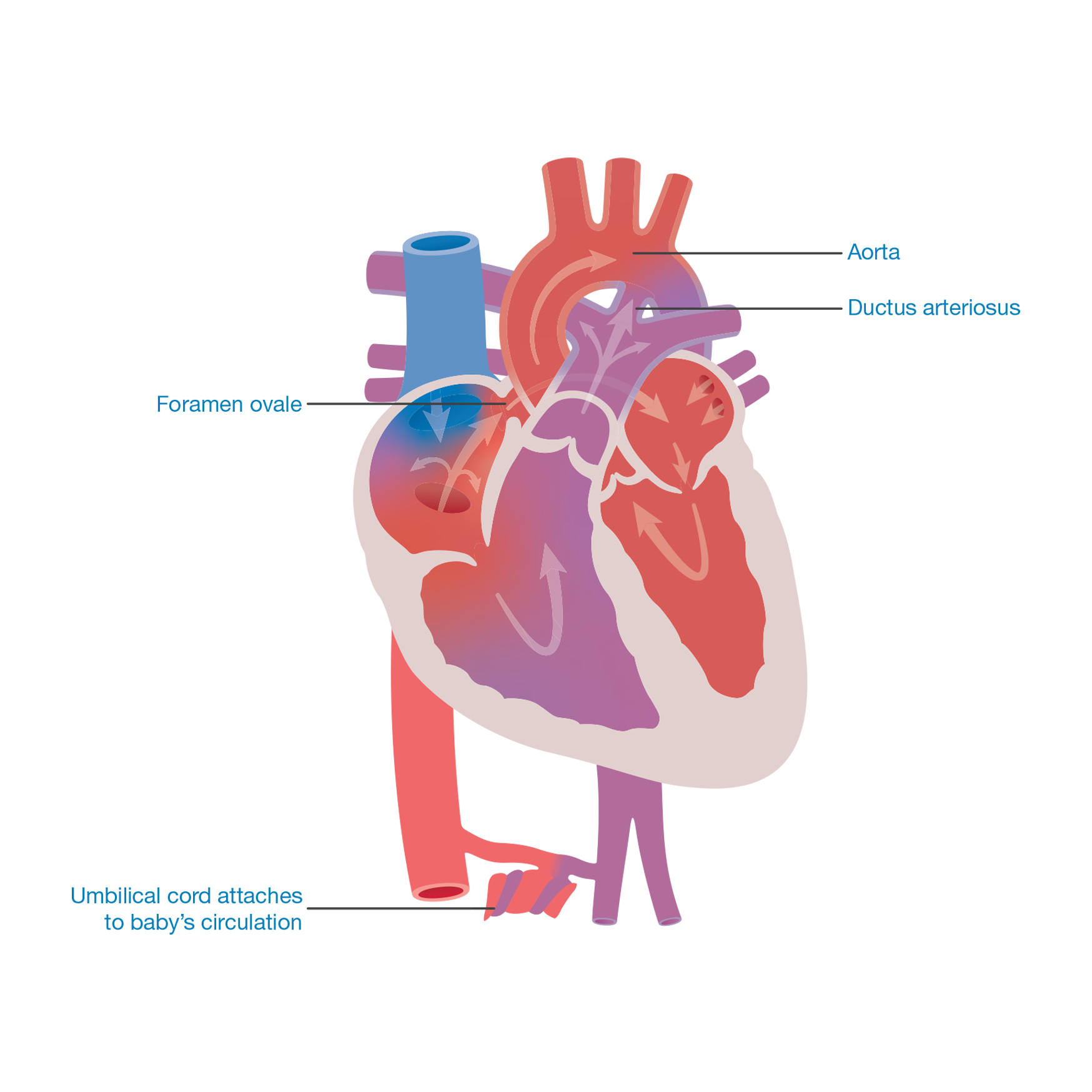
When the baby is still in the mother’s womb it does not need to breathe for itself as the mother is supplying all the oxygen to the baby via the umbilical cord.
The circulation before birth is different from that after birth. It is designed so that the oxygen-filled blood from the umbilical cord goes to the most important parts of the body, for example, the brain. Very little blood needs to go to the lungs.
The heart has designed a series of bypass systems. There is a hole between the upper collecting chambers (the left and right atria) called the foramen ovale. Some oxygen-filled blood passes from the right to the left collecting chamber then on into the left pumping chamber (left ventricle) which pumps the blood around the body. Some blood continues from the right collecting chamber down into the right pumping chamber where it is pumped up to the lungs, via the pulmonary artery.
The second bypass is a connection between the lung artery (pulmonary artery) and the body artery (aorta). The connection is called the ductus arteriosus (duct). Blood passes from the right pumping chamber (right ventricle) into the lung artery (pulmonary artery). Some of the blood travels through the lungs but most of it flows through the duct to the body artery (aorta) and around the body.
When the baby is born and starts to breathe for itself, the bypass systems are no longer needed. Gradually over the first few days or weeks after birth, the duct (ductus arteriosus) and the hole (foramen ovale) between the upper two pumping chambers will close off and the baby’s circulation will be as described by the heart condition diagnosis (as outlined in the following sections).
What exactly is wrong with my baby’s heart?
A detailed account of each specific heart abnormality (with diagrams) will be discussed with you by the fetal cardiac specialist. For more information, have a look at the section single ventricle heart conditions and their treatments where you will find diagrams and a simple written description of the heart problem. Take the information to future appointments with your medical team, who can use it as a tool to help you gain a greater understanding of the heart problem.
The written information can be a reference point when you go home. It can also be very helpful when trying to explain the heart problem to family and friends.
Click here to read our updated information explaining single ventricle heart conditions and their treatments.
Why has my baby got something wrong with its heart?
The baby’s heart is being formed at around the fifth week of a pregnancy, just at the stage when you realise you are pregnant. In most cases it is impossible to give a specific reason for there being a heart defect. In the majority of cases the reason is not currently known.
However…
There are a number of factors which are known to increase the risk of having a baby with a heart problem, such as:
- A history of previous children, either parent or other family members having had a congenital heart problem (heart problem that the baby is born with).
- There may be a fault in the baby’s genetic make-up which has caused the heart defect (See genetics information further down).
- Diabetes in the mother, particularly if poorly controlled.
- Illegal drug abuse or serious alcoholism.
- Some medications such as those used for the treatment of epilepsy carry a small risk of causing heart problems, but are essential for the mother to keep her healthy and well.
- Other problems with the baby, for example, stomach or bowel problems.
Did we cause the baby’s problem?
Parents often worry that they are responsible in some way for the baby’s heart condition, but it is highly unlikely that there is anything you have done or not done which would have caused the problem.
Genetics
Many families who have a child with congenital heart disease ask why their child was born with the condition. In some cases the malformation will have occurred because of a genetic problem that has affected the heart as it formed in the womb.
A blueprint
When a new house is built, the architect draws up a plan of what the house will look like and how it is going to be built. When a new child is being created, information is drawn from the mother and the father to make a plan of how the child will look and how their body will be put together to work.
A genetic blueprint
Every person in the world has a genetic blueprint of their own. The blueprint is stored in every cell in their body and holds the information required to help the body grow, develop and work properly. The information is made up of lots of messages which we call genes. We have about 30,000 genes in each cell of our body. Different genes carry different messages that are responsible for instructing our body to do specific things. For instance, genes determine the colour of our hair or eyes or how cells work in different organs, for example, the liver, heart or lungs. The genetic blueprint is our very own information computer.
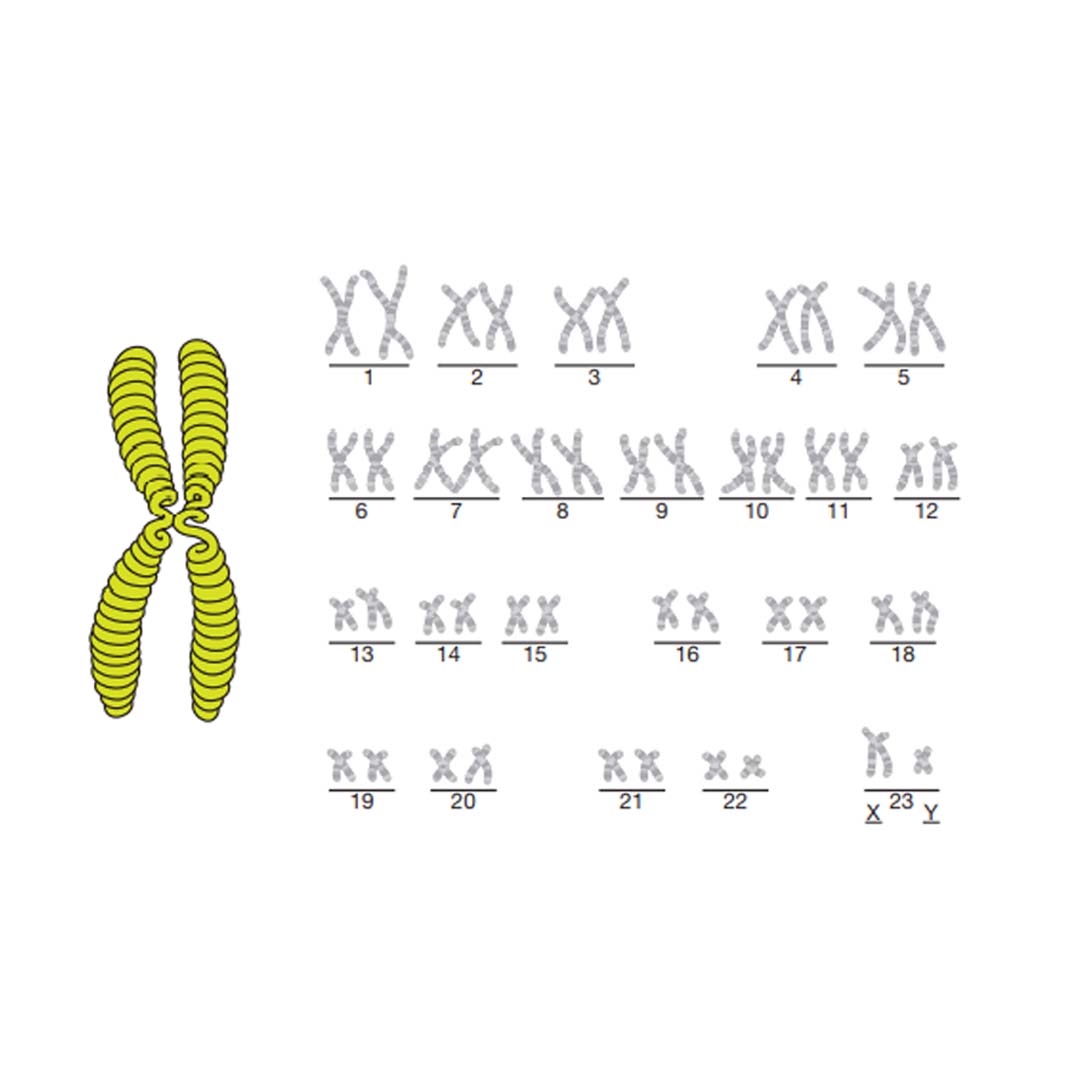
The genes are stored in coils and split into chromosomes (see the diagram on page 16). Humans have 23 pairs of chromosomes, so 46 in total. 23 chromosomes (one of each pair) come from the mother and the other 23 from the father. They are transferred in the egg and the sperm that make a child.
The picture on page 16 shows what the chromosomes look like – if you look at the last set of chromosomes in this picture you will see that they are labelled X and Y. These are the chromosomes that 16 decide if you are male or female. The chromosomes picture must represent a man because there is an X and a Y chromosome. A woman always has two X chromosomes. The sex of a baby is determined by which chromosome comes from the father: X for a girl, Y for a boy.
Genetics and heart disease
Some congenital heart conditions are linked to a genetic disorder such as Edwards’ syndrome or 22q Deletion. These disorders are caused when one of the 46 information chromosomes is malformed. As the baby grows in the womb, the genetic malformation will cause a particular part of the heart to develop incorrectly. In some cases the genetic condition can be detected before birth.
Geneticists (genetics doctors) are always looking for genetic causes for congenital conditions; however, there are many heart conditions that do not have a specific genetic cause. Many of the single ventricle heart conditions fall into this group.
There may be many factors, as yet unknown, that cause a baby’s heart to develop abnormally. The problems can occur early in pregnancy as the heart forms (before three months) or later as the heart grows.
Congenital heart conditions occur in 1 in 130 pregnancies.2 If you have previously had a child with a single ventricle heart condition the risk of it happening again rises to between 5 and 8%.3 There is also a risk to any pregnancies in the person with the condition and their brothers and sisters. Although the risk is higher, over 90% of future babies will have no problems with their heart.
What further tests will we need?
When any abnormality is found in a baby, it always raises the question whether it has been caused by a problem with the baby’s chromosomes (genetic make-up).
Many families who have a child with a congenital heart problem ask why their child was born with the condition. In some cases the malformation will have occurred because of a genetic problem that has affected the heart as it formed in the womb.
Tests available
There are currently three diagnostic tests available which look at the baby’s genetic make-up:
Chorionic villus sampling (CVS)
Taking a sample of the placenta. This is offered in early pregnancy, and would be relevant for expectant mothers with an increased nuchal translucency measurement (a measurement of a skin fold seen on the neck of the baby).
Amniocentesis
Taking a sample of fluid from around the baby.
Fetal blood sampling
Taking a sample of blood directly from the baby.
All of these tests carry a risk of miscarriage and it is therefore extremely important that parents are encouraged to think through the implications of what they would do with the additional information.
Talk to your midwife or obstetrican to see what would be the most appropriate test, if any, for you.
Chorionic villus sampling (CVS)
- This test is used in early pregnancy when an increased nuchal translucency measurement has been found.
- The miscarriage rate is 1%.
- A fine needle is guided, by scan, through the abdominal wall into the placenta where a small sample is removed.
- An initial result will be available within two to three days and looks for the three major chromosome abnormalities: Down’s syndrome, Edwards’ syndrome and Patau’s syndrome.
- The complete test results will take one to two weeks.
Amniocentesis
- This is the most commonly used diagnostic genetic test. It has a miscarriage rate of 1%.
- A fine needle is guided, by scan, through the abdominal wall into the uterus where a sample of fluid from around the baby is taken.
- The skin cells shed by the baby into the fluid are grown (cultured) and examined to give the chromosomes (genetic make-up) of the baby.
- An initial result will be available within two to three days which looks for the three major chromosome abnormalities: Down’s syndrome, Edwards’ syndrome and Patau’s syndrome.
- The complete test results will take two to three weeks.
Fetal blood sample
- This test has a miscarriage rate of 1%.
- A fine needle is guided, by scan, through the abdominal wall into the uterus where a sample of blood is taken from the umbilical cord or from a small blood vessel in the baby’s abdomen.
- Fetal blood sampling is less commonly used to test the baby’s genetic make-up, but sometimes your medical team may say it is their preferred test.
What is the advantage of having a test?
Every couple will need to think through the reason why they might choose to have a test. Some considerations are explored below.
Some parents feel that they need to know whether the heart problem in their baby is part of a genetic syndrome, such as Down’s syndrome, as this additional information may help them choose the way forward.
There are certain serious genetic conditions which may mean that the baby will not survive pregnancy or live for long after birth and parents may be advised that the option for surgery would not be in the baby’s best interest.
For some parents, knowing their baby has a genetic syndrome in addition to a major heart abnormality may help them with the difficult decision of whether or not to continue with the pregnancy or consider comfort care (palliative care) after birth.
Other parents choose to have a genetic test in order to obtain as complete a picture of their baby’s problems as possible, so that they can prepare themselves and their families during the remainder of the pregnancy.
Possible treatment choices
Having explained your child’s diagnosis, the doctor will go on to discuss what treatments are available. None of these treatments provide a long-term cure but, for many children, they can offer a reasonable quality of life.
It is vital that parents are fully included in the treatment discussions and decisions taken for their child.
These treatment options may include:
Surgical treatment
The aim of this treatment is to re-route the blood through the right side of the heart, bypassing the blockages on the left side. This surgery is offered in three stages over three or more years and involves extremely high-risk open-heart surgery. Your doctors will explain the risks for your child. Even after all the surgery has been performed, your child’s heart will not look normal or work normally, and it may be that it will gradually fail and your child may need a heart transplant in teenage years or early adult life. More information on the surgery follows.
Supported comfort care
As the long-term outcome is unclear for children with Hypoplastic Left Heart Syndrome, it is important to know that there is the option not to put a child forward for surgery. The baby is allowed to die peacefully either in the hospital or at home; the family would be fully supported by hospital and community nursing and medical staff.
Transplantation
Heart transplantation is one of the possible treatments for single ventricle heart disease, but it is not offered as a first treatment within the United Kingdom for the following reasons.
There are very few donor hearts small enough for a baby available in the United Kingdom.
Transplanted hearts do not last for ever and there are many risks involved throughout the recipient’s life. Offering surgery as a first treatment path and retaining transplant as a future option offers a greater chance of a longer life for a child.